OVULATION INDUCTION
IN IRAN
Effective yet affordable ovulation induction procedures
at the best fertility clinics in Iran help your body work
normally to produce enough eggs for natural pregnancy.
Effective yet affordable ovulation induction procedures
at the best fertility clinics in Iran help your body work
normally to produce enough eggs for natural pregnancy.
Suffering from infertility because of ovulation disorders? We at AriaMedTour help you get the most effective ovulation induction treatment at modern fertility clinics in Iran. To get a free consultation and price quote for ovulation induction treatment in Iran, contact us or fill out the above form, and to learn more about ovulation induction, continue reading.
Hear about our patients’ experiences in Iran: They have so much to share.
Watch these stories from different patients around the world to see why people choose Iran for their cosmetic surgeries and how AriaMedTour facilitates their medical trip to Iran.
A medical trip documentary:
Crossing borders for a unique beauty adventure
Having Experienced a Failed Plastic Surgery,
Pakistani Girl Chooses Iran for a Perfect Revision
Beauty Redefined: A Cosmetic Surgery
Journey to Iran – AriaMedTour Documentary
A Smooth Medical Trip to Iran
for an Amazing Transformation
Swiss Patient Trusts Iran for
His Cosmetic Surgery Among All Destinations
Australian Lady Saves Money Having
Successful Plastic Surgeries in Iran
Croatian Girl’s Careful Research Led Her
to Iran for an Amazing Plastic Surgery
A Medical Trip to Iran Is Worth It as You Enjoy
Both Great Surgery Results and Low Prices
Haven’t decided yet? Let us help you, it’s free
Some women ovulate infrequently or do not ovulate at all. Irregular ovulation or anovulation (not ovulating at all) results in irregular periods. These can have a number of reasons but the major ones are stress, weight fluctuations and PCOS (Polycystic Ovarian Syndrome). Thyroid and pituitary gland disorders raised prolactin level, and ovarian failure are some of the other reasons for not having regular ovulation. Ovarian failure may happen as a result of cancer treatment or menopause.
Therefore, when a woman is not ovulating by herself and if she is in a childbearing age and she is not developing mature follicles every month or does so but not as regular as other women, it might be impossible or very tough for her to get pregnant. Aside from that, irregular periods have a big impact on a woman’s mood, sleep, hair, skin and generally on her daily life quality. This is where “ovulation induction” is recommended to the person suffering from this condition.
To determine the follicles development, a pelvic ultrasound is performed to reach the endometrium (lining of the womb). Blood tests may also be done to measure hormone levels to identify a woman’s most fertile time of the month (a time when a woman is most likely to ovulate every month).
In order to successfully treat ovulation problems, the root cause must be identified. To this end, several blood tests and an ultrasound of the womb must be done. With the blood tests, the levels of thyroid hormones, prolactin, FSH, testosterone and other androgens (male hormones) must be measured. The ovary must be also evaluated in order to see whether it is capable of responding to the treatment or not. High concentration of FSH (FSH>10) and low AMH concentration at the beginning of the period, is indicative of a probable ovarian failure. In such cases, the treatment will not be useful, so if anovulation and oligoovulation are secondary to another disease, the “ovulation induction” treatment will not work unless the root cause is taken care of.
The following are candidates for ovulation induction:
These women can benefit from ovulation induction to increase the number of times they ovulate during one cycle to give them better chances to conceive and get pregnant.
There are several methods for ovulation induction, depending on how responsive are the ovaries to each method.
The methods are as follows:
Ovulation induction is induced with one of the following drug regimens:
How does Clomiphene citrate work?
Clomid, also known as Serophene or its alternatives (Tamoxifen and Letrozole tablets) increases the follicle stimulating hormone (FSH) and Luteinizing (LH) production by the pituitary gland. Clomiphene works by tricking the body into thinking that it is deficient or low in estrogen. The pituitary gland sends signals to the ovary, after getting impulses from higher centers in the brain, to stimulate the development of the follicles and eggs growth. An LH surge will happen a few days after stopping taking clomiphene citrate, and 36 hours after this surge the patient will start to ovulate.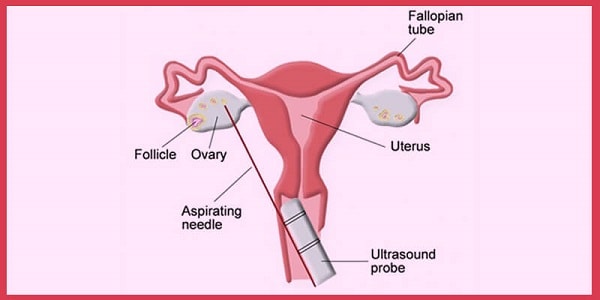
This tablet is usually given at a starting dose of 50 mg for 5 days of a cycle, usually starting from the second day of the period. Although FDA has approved of a daily intake of 125 mg, the dose will only be increased if the patient does not respond to 50 mg dose and they fail to ovulate; as a result, it will be increased to 100 mg per day. If periods are very irregular and infrequent, in order to induce periods, another tablet regimen might be needed. This tablet is called Norethisterone.
How effective is Clomiphene citrate?
The effectiveness of Clomid is dependent on a number of reasons, such the age, infertility issues and seminal parameters.
If a pregnancy is achieved with clomiphene citrate, the chances for twins is about 6- 10% and for triplets or higher is 1% or less.
Clomiphene side effects
Clomiphene citrate usually has no immediate serious side effects, but blurred vision, hot flushes, and mood swings may happen.
How does Gonadotropins work?
This is an injective method of ovulation induction. An injection is done with a small needle daily. These daily self-injections must be continued for 5-12 days. The starting dose varies from patient to patient in order to optimize the probability of conceiving and reduce the chances of multiple pregnancies. The right dosing will be adjusted by monitoring the patient with ultrasound and hormonal evaluation. This injection works by maturing the eggs inside the follicle. Afterward, with an HCG injection which mimics mid-cycle physiologic LH surge, ovulation will happen.

Gonadotropin injection is an ovulation induction method that is continued for 5-12 days.
Gonadotrophins are known with these trade names:
If pregnancy is achieved with this method of ovulation induction, the chances for twins is about 15%, for triplets it goes down to 5% and more less than 1%.
HCG, also known as Novarel, Profasi or Ovidrel is used as an injective ovulation induction method when there are sufficient amounts of matured follicles. With ultrasound, it’s easy to keep track of how responsive is the patient to the drugs. It can then be possible to know when the follicles have grown to their appropriate size, when intercourse is advised and HCG injection might be needed to help with the timing of intercourse or IUI (the process of transferring the semen directly into the uterus). Each patient has different responses to the ovulation induction. The response might be either too strong or not sufficient. In such cases, the current cycle may need to be canceled and a new one will need to be started. If the response turns out to be satisfactory, the treatment can be continued for another 6 consecutive cycles, without break and interruption.
Letrozole, also known as Femara, is an oral ovulation induction method. Although this method has not been approved by the FDA, it can be used as an alternative to Clomid (clomiphene citrate), as it has the same results as Clomid. If a patient suffers from Clomid’s side effects, she can alternatively use Letrozole. The starting dose is 2.5 or 5.0 mg, if ovulation does not occur, the dose will be increased by 2.5 mg. Most doctors will not exceed 7.5 mg.
GnRH analogs, also known as Lupron, Leuprolide Acetate, Ganirelix, Antagon or Cetrotide are similar to GnRH. To control the pituitary gland, GnRH is released by the hypothalamus in the brain. FSH and LH secretion, that are necessary hormones for egg production and subsequent ovulation, is done by stimulating the pituitary gland, which is also a result of a pulsatile release of GnRH hormone. The opposite occurs with synthetic release of GnRH analogs. With Lupron, an FSH and LH suppression happens after an initial increase in those hormones. With Antagon and Cetrotide, immediate suppression might happen. Using GnRH analogs simultaneously with Gonadotrophrine treatment allows for better hormonal control and guarantees more successful results with less failed cycles.
Women with PCOS who do not ovulate or do not ovulate regularly may be treated with Clomid at first, which in most cases has a satisfactory response. But there are two other options to consider:
PCOS is known for affecting insulin and glucose metabolism. Metformin is a medication used in Diabetes treatment, which on the other hand improves ovulation in some patients with PCOS.
This is surgical ovulation induction method. In this method about four 4-mm length holes are drilled in the ovary. This method needs laparoscopy and helps women with PCOS to ovulate in 60% to 85% of cases. Scarring rarely happens in this invasive procedure, but it carries the risks of laparoscopy, which are often minor and the serious ones are rare.
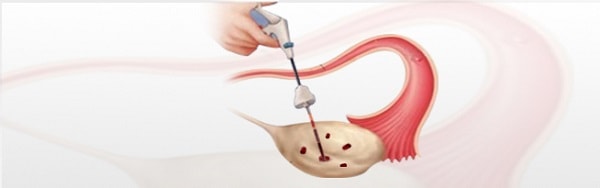
Ovarian drilling is an ovulation induction method suitable for women with PCOS
In Iran, all ovulation induction methods are performed by qualified specialists. For people with PCOS Iranian doctors usually prescribe clomiphene citrate as the first option to help women to ovulate. For patients who are planning to conceive, other methods may need to be performed. In terms of advancement, Iran’s fertility treatment services are in sync with developed countries.
To compare the ovulation induction cost in Iran with other countries, we take the HCG injection as an example. A course of HCG injection costs around …… in Iran, while an average course of HCG injection in the United Staes costs $400 approximately.
Contact Our Medical Support Team: