Reading Time: 7 Min
What are dental implants?
Dental implants are the miracles of dentistry where your not-so-attractive smile can be replaced with a line of pearly white teeth and your lost tooth can be replaced for proper functionality that aids chewing and digestion. They greatly contribute to your beauty and health.
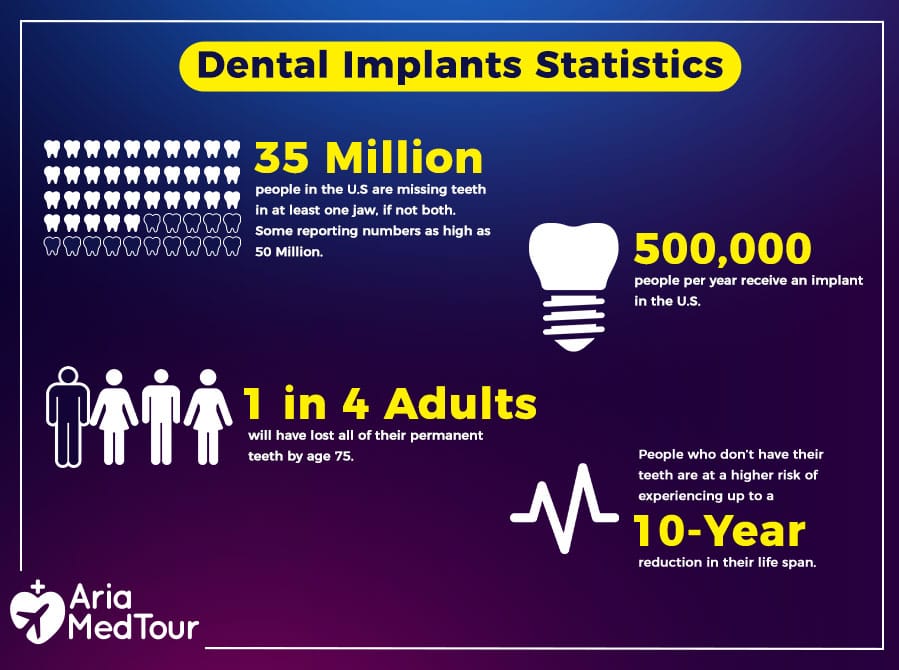
About 70% of adults between 35 and 44 in the US alone have lost at least one tooth due to trauma, dental decay, or gum disease, which can be replaced with an implant with a 95% success rate.
Dental implants are made from 2 parts, one of which acts like the root and the other is the crown. The former is a screw-like structure often made from titanium that will integrate with your jaw bone. If you have experienced bone loss, a bone graft will be necessary to strengthen the foundation for the implant. During the next 3-6 months, your bone will regrow to hold the implant in place. After complete healing, the crown will be placed, which is often made from ceramic.
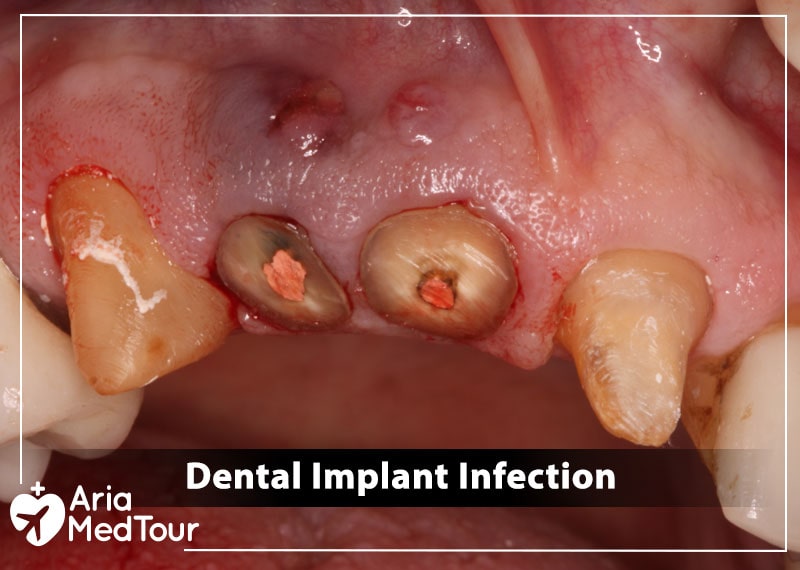
What is dental implant infection?
Dental implant infection is relatively rare but it starts with the buildup of bacteria that is neglected. It gradually develops to peri-implant mucositis which involves soft tissue (mucosa) inflammation. If it is not treated promptly, it will turn to peri-implantitis, which is a gum disease involving both soft and hard tissue, leading to bone loss and implant failure. If still neglected, it will lead to a systematic illness that is harder to treat and damages other organs.
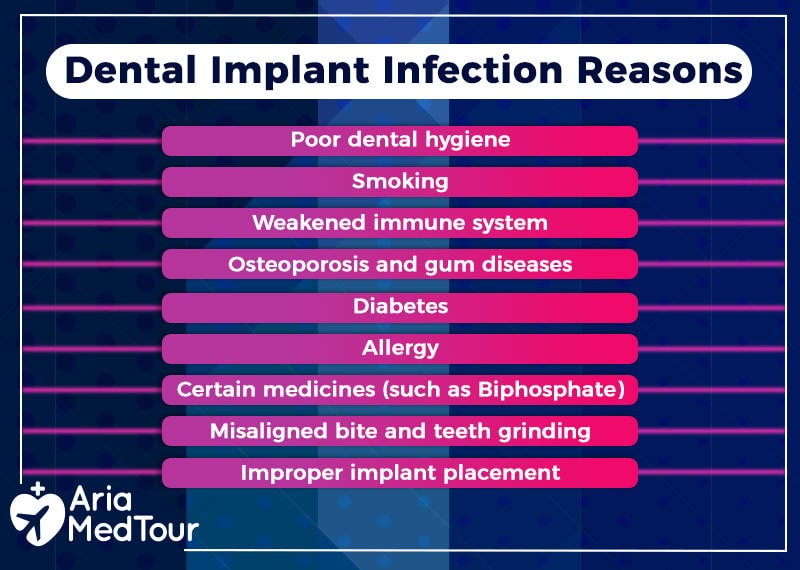
Why does dental implant infection occur?
Just like your natural teeth, dental implants can get infected because bacteria can grow and create a plaque that affects your gum and the underlying bones. Often a plaque biofilm is formed between the titanium implant and prosthetic crown that gradually extends to the gum.
Dental implant infection might occur due to many factors including the following:
- Poor dental hygiene: Lack of proper oral hygiene is the most contributing factor that allows the bacteria to stay and build up.
- Smoking: Smoking reduces blood flow to the gum due to blood vessel restrictions, which hinder nutrient delivery and removal of waste products. It also introduces bacteria to the mouth, which increases risk of buildup and infection.
- Weakened immune system: A compromised immune system for any reason can greatly impact the body’s ability to fight bacteria, which can eventually lead to infection.
- Jaw and gum conditions: Osteoporosis and gum disease (periodontitis) can also cause dental implant infection as they create gradual bone loss.
- Diabetes: Some diseases such as diabetes can also lead to infection as they cause systematic disruption in metabolism and the immune system.
- Allergy: Allergic reaction to implant itself might be a contributing factor.
- Certain medicines: Medications such as biphosphate for cancer are also considered a cause.
- Malocclusion or parafunctional habits: Misaligned bite (crossbite, overbite, underbite, open bite) and teeth grinding (bruxism) can eventually cause bacteria buildup and tooth implant infection.
- Improper implant placement: Surgical technique is very important in a dental implant procedure to make sure proper sterilization is observed and there is no gap left between the implant and jaw bone for the bacteria to grow. A highly qualified dentist with extensive experience in dental implants will take any measure necessary to prevent any chance of infection.
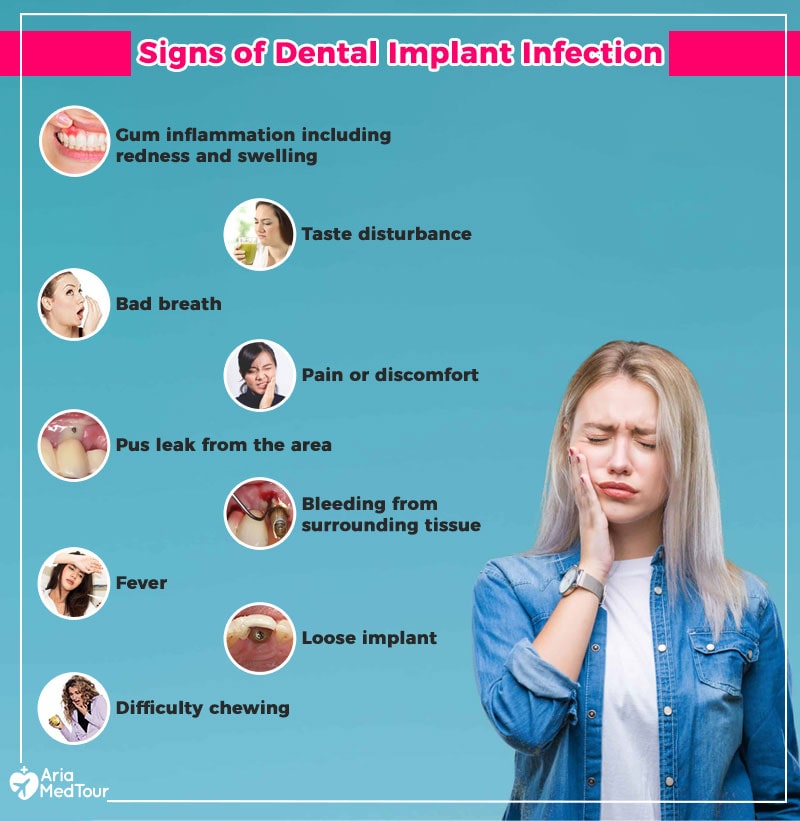
What are the Signs of dental implant infection?
Dental implant infection is just like natural tooth infection that causes the following symptoms:
- Gum inflammation including redness and swelling
- Taste disturbance
- Bad breath
- Pain or discomfort
- Pus leak from the area
- Bleeding from surrounding tissue
- Fever
- Loose implant
- Difficulty chewing
In case of noticing any sign of infection, contact your dentist immediately and follow the instructions. If left untreated, a simple inflammation can lead to systematic infection with severe consequences.
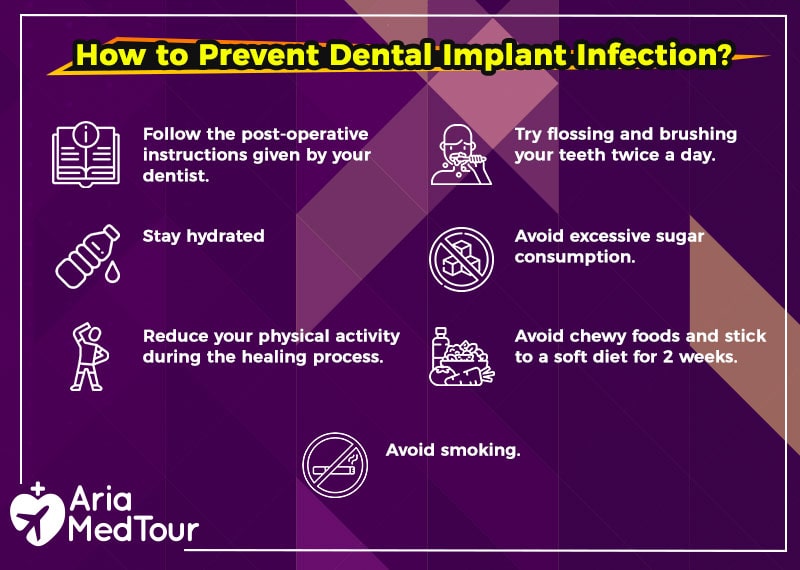
How to prevent dental implant infection?
Prevention is the key to implant success, which is simple if you start immediately after your surgery:
- Follow the post-operative instructions given by your dentist. They are designed according to your individual needs so you must stick to them rigorously.
- Keep up with a routine dental hygiene that includes flossing and brushing your teeth twice a day. Be gentle though.
- Stay hydrated as water can flush bacteria buildup.
- Avoid excessive sugar consumption including drinks and fruit juices.
- Reduce your physical activity during the healing process.
- Avoid chewy foods and stick to a soft diet for 2 weeks after implant surgery such as soups, smoothies, yogurt, cottage cheese, oatmeal, mashed potatoes, scrambled eggs, bananas, and applesauce.
- Avoid smoking as it reduces your dental implant chance of success by 10%.
- Have your implants checked and cleaned by your dentist twice a year.
How to treat dental implant infection?
The treatment aims to stop the progression of infection and to maintain the implant. It starts with an accurate diagnosis based on X-ray imaging to determine any possible bone loss. Then periodontal probing will determine the stage of infection and a treatment plan will be recommended which include a combination of the following methods:
-
Antibiotics
They are the first line of defense against any infection that might include pills or prescription-strength mouth rinse. Sometimes antimicrobial therapies are prescribed for infections caused by other microbes.
-
Mechanical debridement
This method is appropriate for shallow mucosal pockets where a carbon fiber curette or an ultrasonic device is used. Also known as submucosal debridement, the high-frequency waves clean the infected area around the implant.
In the case of deep mucosal pockets which are more than 5mm, mechanical flossing or delicate scaling instruments are used to clean the contamination without damage to the surface of the rod. Localized antiseptics are often used after mechanical removal of the infection.
-
Surgery
A surgical method or open flap debridement is utilized when access to infection site is not possible so a flap of gum is opened. According to the need, mechanical debridement and antiseptics are also combined.
-
Laser surface decontamination
This is a recent approach where laser beams are used to remove contamination from the surface of the titanium implant and surrounding tissues. The pulse settings are adjusted according to the level of peri-implantitis.
-
Implant removal
This is the worst-case scenario when the level of infection is severe and bone loss is significant which often happens when peri-implant mucositis develops into deep peri-implantitis. Surgical instruments such as a trephine or a forceps are often used for this procedure.
After several months of healing and bone grafts, reimplantation might be an option.
You May Like to See Before & After Photos of Dentistry
You May Like to See Before & After Photos of Dentistry
Final words
Dental implant infection is rare but easily preventable. You have the power to prevent dental implant infection when you follow the aftercare instructions and daily hygiene routines given by your dentist. However, choosing a highly experienced dentist is also important to prevent infection because the surgical technique can minimize any chance of bacteria growth.
No matter what the cause is, dental implant infection is easily treatable if diagnosed in the early stages. It is just like any other infection risk that is associated with any kind of surgery.
In case of any sign of inflammation, even slight redness and pain, visit your dentist immediately for a professional checkup and treatment.
Dentistry Packages
Surgery + Hotel + Visa
Transfer + Interpreter
Related Articles
Share this article:
Feel free to express your opinions or ask your questions regarding the article















I think I might be dealing with a dental implant infection, but I’m not completely sure. Are there specific dental implant infection symptoms I should watch out for? I’ve seen some dental implant infection pictures online, and it made me more anxious. How do I know if what I’m experiencing is serious?
Hi Caroline! It’s completely understandable to feel concerned. Common implant infection symptoms include persistent swelling, redness, pus, bad taste in the mouth, and increasing pain around the implant site. While dental implant infection pictures online can give you a general idea, only a dentist can confirm whether it’s actually infected. If you notice these symptoms, it’s best to seek professional evaluation as early diagnosis leads to more effective dental implant infection treatment.
I’m studying oral health and came across several cases of dental implant infection. I’m curious — once an infection starts, what is the recommended dental implant infection treatment? And do the implant infection symptoms always appear right away, or can they develop slowly over time?
Hi Samuel! Great questions. Dental implant infection symptoms can appear within days or sometimes develop gradually over weeks, depending on the cause. Early dental implant infection treatment usually involves antibiotics, deep cleaning around the implant, and removing infected tissue. In more advanced cases, the implant may need to be temporarily removed so the area can heal. Recognizing implant infection symptoms early significantly improves the success of saving the implant.